Introduction
The prevalence of diverticular disease has increased over the past few decades, with estimates of up to 2/3 of the general Western population above 40 years of age currently being affected [1-5]. Possible explanations for the increase in prevalence are increased aging, dietary habits and an increase in average body mass index [6].
Most people with this abnormality go unnoticed, but complaints can occur. Diverticulitis leading to clinical symptoms is the most common complication of diverticular disease. This affects approximately 10-25% of the population with diverticular disease, elsewhere, a lower incidence also has been reported [4,7,8].
Another complication is bleeding mostly due to the concomitant use of anticoagulant therapy. Subsequently diverticulitis composes a major health burden and results in 18.000 yearly hospital admissions in the Netherlands [9]. Diverticulitis is a clinical diagnosis based on a combination of clinical features such as abdominal pain (especially in the lower left quadrant), changes in defecation pattern, pain on physical examination, leukocytosis and high CRP. The diagnosis is generally confirmed by a radiological examination. Currently, CT-scan is considered as the gold standard, with a sensitivity and specificity of 93% and 97% [10]. Moreover, CT-scan
has the added possible benefit of defining disease progression and adverse events such as abscess formation, fistula, obstruction or perforation. Ultrasound may also be used, with reported sensitivity and specificity ranges as high as those obtained by CT-scan in some studies [11-14]. However, the credibility of ultrasound results is highly dependent on the physicians experience and patient characteristics such as the amount of abdominal fat.
It is well-known that diverticuli occur at older age and those concomitant abnormalities like adenomas or even cancer can be present [15]. However, due to overlapping imaging features of diverticulitis with colorectal carcinoma, it has been hypothesized that signs of colorectal cancer might be missed on CT-scan. Several guidelines recommend routine screening for colorectal cancer when the acute phase of diverticulitis has resolved, usually after 6-8 weeks [16-20].
As previous studies have shown conflicting results as to whether patients with diverticulitis have an increased risk of colorectal cancer when compared to the general population, the question of whether colonoscopy should be performed after an episode of acute diverticulitis remains a topic of debate. In normal daily practice elective endoscopic investigation of the colon has low additional diagnostic yield. For this reason a group of consecutive patients diagnosed with diverticulitis was studied in order to gain more information on presence of concomitant abnormalities.
Material and Methods
The study is unique in the sense that the inclusion criterion was not the clinical presentation of the patient but the radiologic diagnosis of diverticulitis.
At the department of Radiology of the Zaans Medisch Centrum, the community hospital of the Zaanstreek region in the Netherlands, all consecutive requests for ultrasound and/or CT-scan of the abdomen in a three year period, from 2016-2018, were studied. Only if the term Diverticulitis was mentioned in the text of the application (either as current differential diagnosis or past diagnosis) the procedure was included. All the selected procedures were meticulously read and if there was diverticulitis diagnosed and mentioned in the conclusion, than this specific investigation was included in the present study.
From each of the selected files the hospital records were searched for the presence of endoscopic investigation of the colon and rectum. This is generally done 6-8 weeks after discharge. If this was not done the reason for not doing an endoscopy was noted. The primary outcome of the study was the prevalence of colorectal carcinoma. Secondary outcomes were the prevalence of polyp (s) (adenomas as well as hyperplastic polyps) and inflammation. Statistical analysis was done with chi-square test for contingency tables and t-test. The alpha level was set at 0.05.
Results
In the three year period 1410 consecutive ultrasound investigation and/or CT-scans of the abdomen were performed. In 1024, procedures diverticulitis! or diverticulitis?, was mentioned in the application (the exclamation mark means that the clinician diagnosed diverticulitis, the question mark means the clinician suspected diverticulitis to be present). These consisted of 390 ultrasounds and 634 CT-scans. After exclusion 198 patients (19.3%) remained with the radiological confirmed diagnosis of diverticulitis. The remainder had other diagnoses or reasons for abdominal complaints.
One hundred twenty seven out of 198 (64%) patients underwent an additional endoscopy (group 1) (6-8 weeks after the acute episode). Seventy one patients (36%) did not undergo a colonoscopy (group 2) after the acute episode. Table 1 shows the demographic characteristics of both groups. There was no difference in gender or in age between both groups.
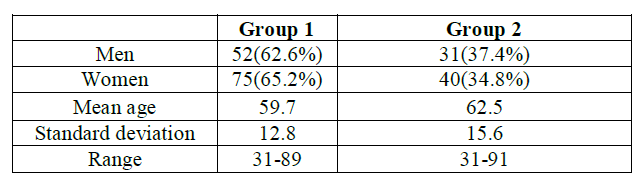
Table 1: characteristics of both groups of patients.
Colonoscopy showed additional abnormalities in 22 (17.3%) of the patients. These were hyperplastic polyp(s) in six, adenomatous polyp(s) in nine, polyps without histological confirmation in three and segmental colitis in three (so-called SCAD = segmental colitis associated with diverticulitis). Eleven polyps were larger than 1 cm, and 10 smaller than 1 cm. Two male patients (43 and 61 years of age) were diagnosed with sigmoid cancer. Both had non-subsiding diverticulitis with abscess formation at the location of the tumor.

Table 2: Reasons for not doing an additional colonoscopy.
Despite the radiological diagnosis, in group 1 diverticuli were not seen during colonoscopy in 8 patients (5 men, 3 women). One additional patient underwent emergency surgery because of fecal peritonitis. Diverticuli were seen in the resection specimen. A post-operative endoscopy showed no more diverticuli. Of the remaining 7 patients one had an undetermined colitis, and another one had a small adenoma. Table 3 presents the laboratory investigation of these 8 patients.
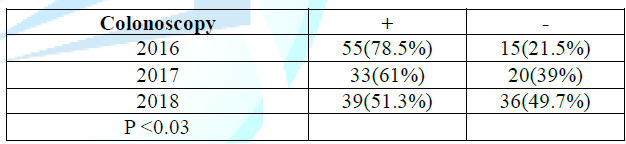
Number 7 was the patients with a sigmoid cancer. In the course of the three years the number of additional colonoscopies decreased significantly (Table 4).
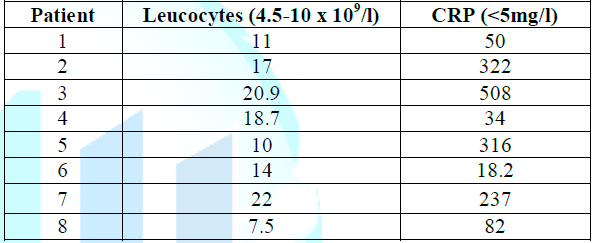
(= normal value).
Discussion
The purpose of the present study was to report on the prevalence of colorectal carcinoma after an episode of image proven diverticulitis in a non-selected population. Colon cancer was diagnosed in two patients (1.6%). During review of the CT-scans of both patients, there were signs that raised the suspicion of a malignancy being present in one patient. However, the radiologist reported diverticulitis as the most likely diagnosis. The other patient underwent follow-up CT-scan because of non-subsiding complaints, which showed persistent inflammation. Afterwards, a malignancy was proven on colonoscopy.
The low percentage of 1.6% of colorectal carcinomas found in our population is consistent with the majority of published research. However, there has been some variability in the percentages reported for colorectal carcinomas and polyps after an episode of diverticulitis. Disbrow et al. reviewed the literature from 1984 to 2015 and reported on two systematic reviews [21]. These reviews indicated a pooled prevalence for colorectal carcinoma in uncomplicated diverticulitis of 1.5% and 0.7% respectively. Moreover, Sharma et al. also reported on complicated diverticulitis and found a pooled prevalence for colorectal carcinoma of 10.8% for this group. [22,23]. As already stated, in the present study both patients with colon cancer had complicated diverticulitis, whereas no colon cancer was found in patients with uncomplicated disease.
The most recent systematic review by Meyer et al. included 31 studies, compromising 50,445 patients, and found a pooled prevalence for colorectal carcinoma of 1.9% [24].
When dividing this population into complicated and uncomplicated disease, a significantly higher percentage of 7.9% was found for complicated diverticulitis versus 1.3% for uncomplicated diverticulitis [24]. Despite this low percentage in uncomplicated diverticulitis routine colonoscopy in all patients after diverticulitis is still recommended.
These results from the literature add to the discussion whether colonoscopy is mandatory after an episode of diverticulitis. Is the incidence of colorectal cancer after diverticulitis higher than with the incidence in the general population? A large study addressing the prevalence of colorectal carcinoma in the general population is by Pox et al.
They report on almost three million screening colonoscopies performed in Germany, and they found a colorectal carcinoma percentage of 0.9% [25]. The prevalence of colorectal carcinoma found in the current study is only slightly higher when than that of the general population. In addition, both patients with malignancy in our study showed that diverticulitis and a colon cancer can be present at the same time.
Thus diverticulitis is not a risk factor for developing colorectal cancer, and that the necessity of performing a colonoscopy may have been exaggerated. Therefore, colonic endoscopic evaluation should be preserved for patients with a higher risk on colorectal cancer. This includes complicated diverticulitis, a protracted clinical course or uncertainty of the diagnosis on CT-scan.
Of course, the present study has several limitations. All cases came from a single center study and not all diagnoses of image proven diverticulitis were followed up with a colonoscopy. On the other hand a large number of these patients had a previous colonoscopy showing diverticuli, and the population under study is a non-selected group from the general population without selection bias.
A recent guideline in the Netherlands does not recommend colonoscopy after a period of uncomplicated diverticulitis [26]. This guideline was published in May 2018, and since then the number of colonoscopies has decreased (Table 4).
In conclusion, previous studies and the data in the present study indicate that it is safe to omit colonoscopy after an episode of uncomplicated diverticulitis. Only in cases of complications or persistent complaints should cancer be part of the differential diagnosis and a subsequent colonoscopy be performed.
References
- Ferzoco LB, Raptopoulos V and Silen W. Acute diverticulitis (1998) N Engl J Med 338: 1521-1526. http://dx.doi.org/10.1056/NEJM199805213382107
- Painter NS and Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization (1971) Br Med J 2: 450-454. https://doi.org/10.1136/bmj.2.5759.450
- Painter NS and Burkitt DP. Diverticular disease of the colon, a 20th century problem (1975) Clin Gastroenterol 4: 3-21.
- Parks TG. Natural history of diverticular disease of the colon (1975) Clin Gastroenterol 4: 53-69.
- Tursi A. Acute diverticulitis of the colon-current medical therapeutic management (2004) Expert Opin Pharmacother 5:55-59. http://dx.doi.org/10.1517/14656566.5.1.55
- Lee TH, Setty PT, Parthasarathy G, Bailey KR, Wood-Wentz CM, Fletcher JG, et al. Aging, obesity and the incidence of Diverticulitis: A Population-Based Study (2018) Mayo Clinic proceedings 93: 1256-1265. http://dx.doi.org/10.1016/j.mayocp.2018.03.005
- Stollman N, Raskin JB. Diverticular disease of the colon (2004) The Lancet 363: 631-639. http://dx.doi.org/10.1016/S0140-6736(04)15597-9
- Loffeld RJ. Long-term follow-up and development of diverticulitis in patients diagnosed with diverticulosis of the colon (2016) Int J Colorectal Dis 31: 15-17. http://dx.doi.org/10.1007/s00384-015-2397-1
- Prismant (2010) Data of hospitalization in the Netherlands.
- Ambrosetti P, Grossholz M, Becker C, Terrier F and Morel P. Computed tomography in acute left colonic diverticulitis (1997) Br J Surg 84: 532-534. http://dx.doi.org/10.1046/j.1365-2168.1997.02576.x
- Puylaert JB. Ultrasound of colon diverticulitis (2012) Dig Dis 30: 56-59. http://dx.doi.org/10.1159/000336620
- Schwerk WB, Schwarz S and Rothmund M. Sonography in acute colonic diverticulitis (1992) Dis Colon Rectum 35: 1077-1084. http://dx.doi.org/10.1007/bf02252999
- Zielke A, Hasse C, Bandorski T, Sitter H, Wachsmuth P, et al. Diagnostic ultrasound of acute colonic diverticulitis by surgical residents (1997) Surg Endosc 11:1194-1197. http://dx.doi.org/10.1007/s004649900567
- Zielke A, Hasse C, Nies C, Kisker O, Voss M, et al. Prospective evaluation of ultrasonography in acute colonic diverticulitis (1997) BJS 84: 385-388. https://doi.org/10.1046/j.1365-2168.1997.02604.x
- Koning MV, Loffeld RJ. A survey of abnormalities in the colon and rectum in patients with haemorrhoids (2010) BMC Gastroenterol 10: 74. http://dx.doi.org/10.1186/1471-230X-10-74
- Andersen JC, Bundgaard L, Elbrond H, Laurberg S, Walker LR, et al. Danish national guidelines for treatment of diverticular disease (2012) Dan Med J 59: C4453.
- Biondo S, Lopez Borao J, Millan M, Kreisler E and Jaurrieta E. Current status of the treatment of acute colonic diverticulitis: a systematic review (2012) Colorectal Dis: The official journal of the Association of Coloproctology of Great Britain and Ireland 14: e1-e11. http://dx.doi.org/10.1111/j.1463-1318.2011.02766.x
- Fozard JB, Armitage NC, Schofield JB and Jones OM. ACPGBI position statement on elective resection for diverticulitis (2011) Colorectal Dis: The official journal of the Association of Coloproctology of Great Britain and Ireland 13: 1-11.
- Jacobs DO. Diverticulitis (2007) N Engl J Med 357: 2057-2066.
- https://www.uptodate.com/contents/acute-colonic-diverticulitis-medical-management
- Disbrow M, Foxx-Orenstein A and Agrwal N. Utility of colonoscopy to exclude underlying malignant polyps after resolution of uncomplicated diverticulitis (2015) J Am Osteopath Assoc 115: 720-723. http://dx.doi.org/10.7556/jaoa.2015.147
- Daniels L, Unlu C, de Wijkerslooth TR, Dekker E and Boermeester MA. Routine colonoscopy after left-sided acute uncomplicated diverticulitis: A systematic review (2014) Gastrointest Endosc 79: 378-389. http://dx.doi.org/10.1016/j.gie.2013.11.013
- Sharma PV, Eglinton T, Hider P and Frizelle F. Systematic review and meta-analysis of the role of routine colonic evaluation after radiologically confirmed acute diverticulitis (2014) Ann Surg 259: 263-272.
- Meyer J, Orci LA, Combescure C, Balaphas A, Morel P, et al. Risk of colorectal cancer in patients with acute diverticulitis: a systematic review and meta-analysis of observational studies. Clin Gastroenterol Hepatol: The official clinical practice journal of the American Gastroenterological Association 17:1448-1456. http://dx.doi.org/10.1016/j.cgh.2018.07.031
- Pox CP, Altenhofen L, Brenner H, Theilmeier A, Von Stillfried D, et al. Efficacy of a nationwide screening colonoscopy program for colorectal cancer (2012) Gastroenterology 142: 1460-1467. http://dx.doi.org/10.1053/j.gastro.2012.03.022
- https://richtlijnendatabase.nl/richtlijn/acute_diverticulitis/follow-up_colonoscopie_na_diverticulitis.html
Citation: Dijkhorst PJ and Loffeld RJLF. Routine colonoscopy after diverticulitis should not be performed to rule out colorectal cancer (2019) Edelweiss Cancer OA 1: 29-32.
Keywords
Diverticulitis, Colorectal Cancer, Sigmoid cancer, Adenocarcinoma, Adenoid cystic, Carcinoma in Situ.


 PDF
PDF